Tēnā koutou katoa
Welcome! Sorry that this one is late on a Friday, but I was hoping for good news about changes to pertussis swabbing and notification processes and so held off sending this through. Unfortunately, it hasn’t yet landed but the first part at least is likely to be sorted very soon. And please note the webinar update on the National Cervical Screening Programme on Tuesday.
Key points today:
-
Pertussis - changes to make pertussis swabbing authorisation and notification process easier are coming
-
Update on radiation oncology services
-
Diabetes complications, and coding in Thalamus
-
Temporary coadministration fee for Boostrix and Influenza
-
Addendum to the last update – Referring to the SCOTS programme
-
University of Otago Primary Health Care Research Prioritisation Study
-
National Cervical Screening Programme (NCSP) Sample Taker Update
-
Upcoming Skin Cancer Courses
-
Introducing our clinical advisors
-
GPNZ Primary Care Clinical Digest – April 24, 2023
What’s new
Pertussis - changes to make pertussis swabbing authorisation and notification process easier are coming
I have been working with public health, microbiology, and laboratory teams locally to try and reduce any barriers to notification of suspected pertussis cases to public health.
-
We expect to stop the requirement for pre-authorisation of pertussis tests in the next few days so that clinicians can test without requiring public health authorisation. It will be important that referrers include appropriate and relevant clinical details, in particular the duration of symptoms, to enable to lab to effectively triage requests. In the absence of appropriate clinical details (in particular around duration of symptoms), requests will be declined by the laboratory and the referrer would then need to contact the lab to provide that information. I will email to confirm when this has been actioned.
-
I am also working with the Public Health team to change the requirement for urgent notification by phone call to public health for suspected cases. This is under constant review. Should incidence of cases or notifications increase significantly (e.g. in a local outbreak situation), then the plan would likely be to move to same day electronic referral (by ERMS). This will be discussed and agreed between primary care and public health, and we will let you know as soon as this change were to come in.
So please be on alert for any further cases of pertussis. Familiarise yourselves with the signs and symptoms of pertussis and how to manage the clinical case (swabbing, isolation and antibiotics) and notification procedures on HealthPathways.
As a reminder, Pertussis, particularly in infants is a serious illness with three deaths reported recently in New Zealand. Any infant showing any symptoms of pertussis should be seen as a matter of urgency and discussed with the on call paediatrician. Also consider individuals that are at high risk of severe illness or complications because of a pre-existing health condition that may be exacerbated by a pertussis infection (for example those with chronic respiratory conditions, congenital heart disease or immunodeficiency, pregnant women…).
Update on radiation oncology services
Radiation oncology services for people living in Otago and Southland continue to be under pressure. Staff from across the country are supporting our local team to minimise the need for patients to travel for treatment, although some patients may need to travel for their treatment whilst we continue to recruit into key Senior Medical Officer vacancies. Over 70% of patients with known responsive cancers with survival benefit or those who have significant symptoms continue to be seen within 2 weeks. Whilst around 50% of all other cancer patients are being seen within targeted wait times.
The Southern Blood and Cancer Service acknowledges this is still not ideal and that any delay in seeing a specialist can be distressing to both patients and their wider whanau. It is reassuring that we continue to have a full functioning treatment team that means for those patients that go on to require Radiation treatment that there is little or no delay in commencing their treatment. We appreciate all those staff working tirelessly to improve this situation and it is testament to the short-term efforts being put in while the longer-term solutions are worked on.
If you have specific queries about your patients, please contact their Cancer Nurse Coordinators cancernursecoordinator@southerndhb.govt.nz via email or on Interim phone support numbers
Dunedin/Otago based:
03 470 9338
027 688 3322
Diabetes complications and coding in Thalamus
We recently analysed microvascular complication rates for people with diabetes in Otago Southland by ethnicity. This was part of Quality Standards for Diabetes Care report that the Local Diabetes Team collates, that WellSouth is part of. A summary is below:
|
|
Māori |
Pacific |
Indian |
Other |
|
Retinal Screening recorded in last 3 years
|
46% |
40% |
37% |
45% |
|
Renal: ACR >30 |
8% |
11% |
3% |
4% |
|
Renal: eGFR <30 |
2.7% |
1.9% |
0% |
1.5% |
|
High risk foot/active foot disease |
15% |
4% |
1% |
4% |
I am sure you will agree with me that there is some work to do for our patients with diabetes, particularly for Māori.
Our Thalamus team are currently working on diabetes coding for all practices as part of trying to improve our diabetes care.
We have noticed that there are patients who are incorrectly coded in our system, which leads to underservicing of diabetic patients and overservicing of patients who have historic reviews but don’t have diabetes.
Our aim is to improve the care of diabetic patients across the board.
We have identified categories where patients are coded incorrectly and have a plan to correct this –
-
Patients who have 2 HbA1c measures in the diabetes range (above 50), but who aren’t coded as diabetic in the PMS. This may have come about through testing outside of Primary Care.
Action: WellSouth will notify you of the names of these patients so they can be coded as having diabetes and be included in annual diabetes review processes.
-
Patients who have never had an HbA1c above 50 who are coded as diabetic or have had an annual diabetes review in the past so are currently counted as a diabetic.
Action: WellSouth will notify you of the names of these patients prior to removing them from our diabetes database, so you are able to scrutinise their notes and see if there is a reason they have been coded diabetic. We would ask you to remove their current diabetes classification too.
-
Patients who have had diabetes in the past (including those with gestational diabetes or those who have had weight loss surgery), who do not currently fit the criteria.
These patients may simply need an annual HbA1c.
Action: WellSouth will notify you of the names of these patients. If you concur we will remove them from our diabetes database. We would ask you to remove their current diabetes classification too, and add an annual HbA1c recall for them
Expect further communication from us that is specific to your practice on which patients fit these categories.
Temporary coadministration fee for Boostrix and Influenza
To support your continued efforts to lift antenatal immunisation rates, there will be a temporary coadministration fee applied when pertussis (as TDaP) and influenza vaccines are administered concomitantly to a pregnant person. This is a temporary coadministration fee paid in addition to the standard administration fee under the Primary Health Organisation Service Agreement (PHOSA).
This temporary coadministration fee will run as a pilot from 1 April 2023 to 30 June 2023 and will include back-dated payments. Success of this pilot will determine if funding can be secured in the future to implement this coadministration fee permanently as part of a wider PHOSA.
Please see the attached letter for full details.
If you have any questions, please contact Olivia Haslam at Olivia.Haslam@health.govt.nz
Addendum to the last update - Referring to the SCOTS programme
In the last update we included information about the SCOTS programme, an innovative orthopaedic programme for patients with persistent knee or shoulder pain (in Dunedin and surrounding area) with a substantial reduction in requirement for people to be assessed for joint replacement subsequently. The Healthpathway will be updated imminently.
However, we left out the key piece of information – being how to refer to the programme.
You can refer to the programme via ERMS: Orthopaedics-Orthopaedics Dunedin Public Hospital-Attention: SCOTs Programme
We continue to advocate for this service to be expanded to other parts of Otago and into Southland.
Opportunities to be involved
University of Otago Primary Health Care Research Prioritisation Study
What are the most important research questions in NZ primary health care?
Your perspectives are important to us.
Survey link: https://otago.au1.qualtrics.com/jfe/form/SV_dp5Z0jD0jVu1WAu
Primary health care providers/academics are invited to participate in a research prioritisation study.
To ensure the research undertaken by the Primary Care Research Network (PCRN) is fit-for-purpose, we are inviting PHC providers and academics to help set the research agenda. Separate projects will focus on Māori community interests, and a patient panel is planned.
This project aims to generate specific research questions that are feasible, highly relevant to PCRN stakeholders and prioritised by their potential to impact health equity in terms of resource allocation and health outcomes. The project has been awarded funding from Health Research South.
Participants will be asked to complete two online surveys. Each round will take around 10 minutes. You will be asked to identify the most important research questions in PHC that need addressing to improve health equity.
The first survey will generate the research questions, and the second survey will rank the curated research questions. Participants will then be invited to participate in an optional meeting (face-to-face or online) which may take 1-2 hours.
For more information about the study, please see the information sheet.
Participants wanted for this study:
(1) Primary health care providers working in Southern Aotearoa, including Māori and non-Māori general practitioners, nurses, nurse practitioners, community pharmacists, community physiotherapists, community dentists, midwives, etc.
(2) Primary health care academics working in Aotearoa, including Māori and non-Māori academic staff based in primary health care/general practice departments, the Schools of Pharmacy, Physiotherapy, Dentistry, Nursing, etc.
If you have any concerns, please feel free to contact Dr Jing-Ru Li (Jingru.li@otago.ac.nz) or Dr Sharon Leitch (project PI) (sharon.leitch@otago.ac.nz).
Please take this link to the online survey:
https://otago.au1.qualtrics.com/jfe/form/SV_dp5Z0jD0jVu1WAu
Upcoming training and webinars
National Cervical Screening Programme (NCSP) Sample Taker Update
9am - 10.15am, Tuesday 2 May 2023
Microsoft Teams: Click here to join the meeting
Te Whatu Ora Southern are holding a clinical update on the rollout of HPV primary screening which is due to commence on 26 July 2023. They want to engage with all sample takers, inclusive of GPs and Nurses, HCAs involved in the recall process etc.
Clinical Update Programme:
9am – Welcome and Housekeeping
9.05am – Southern NCSP Team update
9.15am –HPV Primary Screening Update, Presented by Christy Lange – NCSP Senior Relationship Manager and Alicia Blaikie – NCSP Clinical Advisor
9.45am – Question Time. If you have any specific questions, you would like answered, please email them to cervical.screening@southerndhb.govt.nz before Friday 10 March 2023.
10.15am – Finish
Attendance certificates will be available on request following the presentation. For any further queries please email cervical.screening@southerndhb.govt.nz.
Upcoming Skin Cancer Courses
Skin Cancer Study Day for Nurses
Friday 16 June 2023
Ko Awatea Centre, Middlemore Hospital, Auckland
For primary and secondary care nurses and nursing students, this study day will provide an overview of skin cancer prevention, early detection, treatment and care. Increase your understanding of the journey of a skin cancer patient and the critical role of a nurse throughout this journey, network with colleagues across the region and foster new connections. The cost of attending is $85.00.

Non-Melanoma Skin Cancer Seminar
Saturday 17 June 2023
The Spencer Hotel, Takapuna Auckland
Each year in New Zealand more than 90,000 New Zealanders are diagnosed with one or more non-melanoma skin cancers, and incidence rates continue to rise. Hosted by MelNet with support from NZ Skin Cancer Doctors, this one-day seminar will improve your understanding of the prevention, clinical and dermatoscopic diagnosis and best practice management of common and rare non-melanoma skin cancers. If you’re a health professional with an interest in skin cancer, you won’t want to miss this opportunity to expand your knowledge, network with colleagues across the country and foster new connections – spaces are limited so be sure to register early.
Cost: $250 nurses, registrars, students on an approved training programme, allied health professionals, $375 medical doctors.

Other general information
Introducing our clinical advisors
Over the next couple of updates we will be introducing our clinical advisor team at WellSouth. Please feel free to contact them when you have an issue or idea relating to their areas.
Dr Andy Shute, Clinical Advisor and GP Liaison for Southern Hospitals
Kia ora koutou
I’ve been working part-time for WellSouth since 2020 as Clinical Advisor and GP liaison for Southland hospital. Over this time my role has expanded beyond Invercargill, so it felt appropriate to introduce myself to the wider primary care community.
Originally from the UK, I moved to NZ in 2008, completed GP training in Christchurch in 2012, gaining Fellowship in 2015 and have worked as a GP contractor and employee in a number of practices in NZ and Perth, Australia. I moved back to Waihōpai/Invercargill in 2018 and last year became an owner/director at Queens Park Medical Centre where I work 6/10 at the coal face and 2/10 for WellSouth (every Thursday). I’m also a RNZCGP GPEP1 teacher and GPEP2-3+ visiting medical educator for the Southern region. My wife is a Consultant Anaesthetist at Southland Hospital and I have 2 boys at primary school.
My aim in the liaison role has been to foster clinical relationships and build communication between primary and secondary care, with a focus on collaboration. I’ve been providing primary care perspectives to working groups and initiatives while working with secondary care teams to develop greater understanding of primary care systems, expertise, capacity, funding and challenges; I field and communicate concerns and feedback between primary and secondary care, exploring barriers and solutions; I regularly collaborate with hospital departments (both clinical and managerial), Health Pathways and ERMS, and have a strong focus on data and digital processes. Recently I’ve established the Primary Care Colleague referral pathway (shortly to go live) and worked with Dr David Gow on the Transfer of Care policy promoting respectful and appropriate communication from secondary to primary care.
I’ve already met a number of Otago and Central based practices through my college teaching roles and I’m hoping to get to know more practice teams over time; I’m happy to arrange visits to introduce myself, in person or via Teams and I send periodic (not too often, not too long) updates to primary care teams with progress on initiatives, system issues, feedback, personnel changes etc. So, if you have any issues, feedback or questions that you would like support with or don’t have time to manage, or if you’re not sure how to approach a problem, please feel free to get in touch - I’m not the right person to do everything but I might know who that person is. Andy.Shute@wellsouth.org.nz

Dr Susie Lawless, Clinical Advisor
Kia ora,
I work as a Clinical Advisor to WellSouth on the development and clinical applications of Thalamus, along with the fabulous IT guys and Glen Knol, who you may meet as a practice relationship manager. Having a GP in the team gives real-world insight into what would be useful to the clinical team. Any feedback on Thalamus gratefully received! Susie.Lawless@wellsouth.org.nz

GPNZ Primary Care Clinical Digest – April 24, 2023
In this issue:
-
Immunisation Update April 19 2023
-
Change to Book My Vaccine Age Range
-
Book My Vaccine Weekly Tips and Reminder
-
National Immunisation Programme Operating Guidelines
-
COVID Care in the Community – Updated Public Facing Collateral
-
Update for Pharmacists in General Practice week ending April 14 2023
Top Weekend Viewing
Read the full update here.
Covid-19 updates
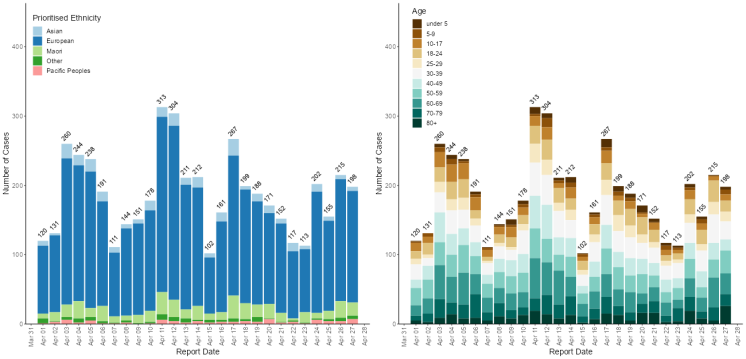
Reported Covid numbers continue to tick on but have dropped back from a couple of weeks ago.
Southern Numbers
Podcast of the Week: Heart Failure: What’s new
This week’s podcast is a really informative update from the Goodfellow Unit on new management aspects of heart failure. Potentially a dry topic, I found it interesting and easy to stay focused listening!
Click here to listen.
So make the most of the sunny weekend ahead, or if youa re catching up with this on Monday, I hope you got a good dose of Vitamin D!
Ngā mihi nui
Carol