Tēnā koutou katoa
Welcome to another full Clinical Director update. Its a good week for new things – the launch of the new cervical screening programme, the naming of our new Long Term Conditions Programme, Toitū Takata, and information about upcoming improvements to the Former Refugee Support programme. We’re also happy to announce that Invercargill people now have the GPSI skin programme available locally. We have just been notified that Whakarongorau Aotearoa staff will be striking this weekend, and the labs will be striking again next Wednesday. And its a month until the elections. Busy times.
Key points today:
-
HPV new screening programme changes
-
Introducing Toitū Takata, the new LTC programme
-
Skin Referral Programme (GPSI skin programme)
-
Upcoming improvements to the Former Refugee Support Programme
-
WellSouth programmes fees update
-
Co-payments and funded programmes
-
Whakarongorau Aotearoa Strike Notice – 15-16 September
-
Awanui Labs Strike Notice – 20 September
-
Aotearoa Immunisation Register (AIR) cut over November 2023
-
Shingrix vaccine first dose
-
Survey: Nursing pay gap – impact on services in the community
-
Update from The Department of General Practice and Rural Health, Dunedin School of Medicine, about changes to the 4th year Medical Students curriculum
-
CHeST Symposium – Emerging Technologies and Health Systems
-
Vaccinating Health Worker (VHW) drop-in session, Thursday 21 September
-
Webinar: The scope and impact of Nurse Practitioners
-
ACC training resources
-
Te Whatu Ora update: in case you missed it
-
Pēpi enrolment survey – last chance
What’s new
HPV new screening programme changes
From yesterday, Tuesday 12th September, the new cervical screening programme kicked off. You will have received info from the Practice Network generic email with all the handy information you need.
This programme will make it easier for patients to get a simple check that not only can make huge differences to your patients in detecting cervical cancer early but makes it easier for you. For many people it will replace a smear. As a result, most people will now only need to screen every five years.
This is the biggest change to one of our core General Practice programmes that has occurred and has the potential to save lives particularly for underscreened women, many of who are Māori and Pasifika.
Some important points to be aware of:
-
Most women and people with a cervix will be moving to 5-yearly screening from their next test. This means their current recall is still valid, and they will need to be screened 3 years after their previous test. If a person is never screened, underscreened or overdue, invite them now.
-
Most screening will be done by patients self-swabbing.
-
One in ten people will need follow- up, a quarter of whom will need referral to colposcopy and three-quarters a LBC (the old style smear) and then followup depending on the result.
-
Screening will continue to be funded through WellSouth for those in high needs groups (Māori, Pasifika, unscreened or under-screened women and people with a cervix, CSC holders). Follow-up testing for all women will be funded now too.
-
Clinicians who are responsible for submitting these screens to the lab will initially be those who are currently authorised to take smears. There is a plan to extend this in the future to all nurses and non-clinical team members.
-
Its all laid out in the new national health pathway, see https://southern.communityhealthpathways.org/20461.htm
You will find attached the short Power Point from the Primary Care drop-in sessions which should answer further questions. HealthPathways hosted a national webinar on the new cervical screening programme last night, and will post the recording next week. There are a few unresolved issues in PMSs, claiming, coding etc that are being ironed out currently. Te Whatu Ora will provide updates when these are resolved through PHOs and their national cervical screening website.
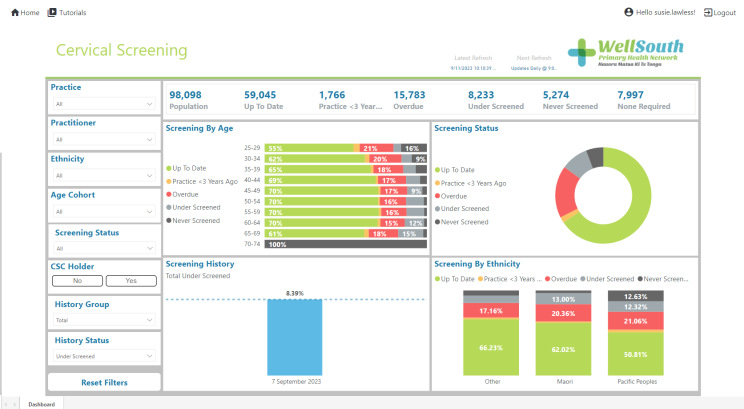
There is a Thalamus page which can list for you all the women who are currently eligible for cervical screening. (See screenshot below of our whole enrolled population). Please use the contact details below for Susie or Glen if you want help with Thalamus. There are nearly 30,000 people in our practices who are overdue, underscreened or never screened. Let’s focus on encouraging these people to come in for a screen.
Codes
We quickly became aware of issues with the CX codes and our team has been working on your behalf along with other PHOs across the country to sort this out!
We are currently talking with the PMS vendor to find a solution, and will contact you as soon as the solution is found.
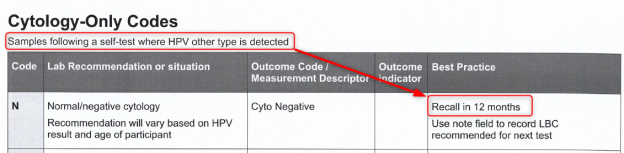
We have also updated the programme sheet.
And attached, are two posters in case you haven’t had a chance to find and print these out.
Questions?
-
Contact your Primary Care Relationship Manager for portal related or claim queries.
-
Your regional contact for the HPV programme on 0800 4 90 70 90 for specific programme queries.
-
For questions about Thalamus, contact Dr Susie Lawless, susie.lawless@wellsouth.org.nz or Glen Knol on glen.knol@wellsouth.org.nz.
Introducing Toitū Takata, the new LTC programme
The new long term conditions programme (replacing CLIC) will be called Toitū Takata.
Toitū is a word used for sustainability, long standing and permanence. Toitū is also a small stream feeding into Otago harbour at the original landing place of Ōtepoti in Dunedin.
Takata is the Kāi Tahu version of Tangata or person.
Essentially the name Toitū Takata means to sustain the people/person and we are proud to be given this name.
Workshops:
In anticipation of Toitū Takata being available in early 2024, WellSouth will offer a series of workshops for Practice Nurses throughout October and November.
These will be aimed at ‘Toitū Takata Nurse Champions’ from each practice and will provide them with the resources to deliver this programme to their patients.
Toitū Takata workshops will be held around the region in October and November. This will be a great networking opportunity and we hope that nurses will attend face to face, but virtual options will also be available.
Please keep an eye on the WellSouth Work Development Calendar for more details.
Skin Referral Programme (GPSI skin programme)
The WellSouth Skin Referral programme is now available for all practices to refer into, including Invercargill.
All skin lesions which meet the criteria in Health Pathways should be referred to this programme as the single point of entry to the service. (If secondary services are required, we will triage and refer on).
We understand that some referrers have experienced frustrations with aspects of the programme and so we have pulled together these tips aimed at helping you and your patient through the service.
Here is a summary of the key points:
-
Anatomical location and close up pictures are essential.
-
Dermoscopic pictures are not required but greatly appreciated.
-
Punch biopsies are only required for NON pigmented lesions.
-
Non pigmented lesions can be referred for excision without prior biopsy but there must be compelling clinical or dermoscopic evidence of malignancy.
-
Referrals must be sent via the WellSouth portal: Skin Lesions Programme – New Referral
More excellent information, in more detail, is here if you click here: Skin referral programme – tips for referrers
Upcoming improvements to the Former Refugee Support Programme
We recognise that providing care to former refugees is complex and time consuming, especially so at the first visit. We also know that at 2 years former refugees are still getting used to the health system in New Zealand, and many are needing ongoing care for long term conditions and trauma related issues.
To recognise this, the refugee subsidy initial visit payment will soon increase from $100+GST, to $160+ GST.
Subsequent visits will continue to be claimable up to a maximum of $80 but we are pleased to advise that the subsidy will be available for 3 years from the date of resettlement (currently 2 years)
We look forward to providing further details once these changes are ready in the WellSouth portal.
WellSouth programmes fees update
We have heard the message it’s been a long time since we have reviewed many of the fees we pay for clinical services that practices provide, and this is something we are actively undertaking at present.
In the last few months we have funded Winter Wellness Checks which was well received by practices and we appreciate practices’ work to support the community.
We have increased Diabetes Annual Review payments for Māori and Pacific people from $40 to $50. We have also provided funded visits for Māori and Pacific people with diabetes who are eligible but not currently prescribed SGLT2 inhibitors or GLP-1 receptor agonists.
The New LTC program, Toitū Takata, is coming on stream in the new year, and there will be separate funding for Advance Care Planning which is coming on stream before Christmas. Changes are also soon to come into place for Former refugees by increasing initial payment and changing the duration from 2 to 3 years, as noted above.
We are about begin a process to resolve the issues we recently identified in palliative care funding. This will be done in partnership with Te Whatu Ora, Aged Residential Care, our hospices and general practice leaders.
Please note that our focus for many of our programmes is on equity as we move forward, which is consistent with WellSouth’s strategic direction and the guidance from Te Whatu Ora where spending needs to be made to address health inequity.
Our Clinical Quality Committee is currently helping provide us with advice about Understanding the cost of time in general practice for both nurses and doctors to provide different types Of care as part of our fee reviews
We are also working in conjunction with other South Island PHOs to compare and standardise - where possible - the fees we pay practices and the services we fund. This is an exciting opportunity to bring more services into our district, as some services that are available in other Te Whatu Ora areas are not available in Southern. A good example of this is the current review of POAC funding at Te Wai Pounamu|South Island Level.
So please know we have heard you, we have made some changes and more is coming.
Co-payments and funded programmes
Please remind your teams that a patient cannot be charged a co-payment if you are claiming for their treatment from a WellSouth funded programme; this includes any POAC service.
Whakarongorau Aotearoa Strike Notice – 15-16 September
Message on behalf of Te Whatu Ora:
Kia ora koutou
Te Whatu Ora has been advised by Whakarongorau Aotearoa that NZNO and PSA members staffing their government funded national telehealth services will strike for 24 hours from 3.00pm Friday 15 September to 3.00pm Saturday 16 September.
The strike will result in significant disruption to contracted telehealth services during this period.
Most services will continue with significant reduction in capacity to answer calls, leading in many cases to longer wait times for service users. Some services will not be available and will divert to automated answer messaging for the duration of the strike.
Available staffing will be prioritised for services that support people in immediate danger. Where possible staff have been assigned to services with greatest risk, but this isn't possible where they are required to hold specific skills of knowledge.
A full list of impacted services will be available tomorrow, along with how the service reduction will be signalled to service users, the alternatives that will offered, and planned system service mitigation during the strike period.
We understand this reduction or removal of key services will likely have significant flow-on effects for other health service providers in the system during this time.
Te Whatu Ora is also reviewing the automated messaging and call management decisions Whakarongorau Aotearoa is planning to use for all affected services to ensure that it aligns with our clinical standards and the mitigation planning we are undertaking with alternative services around the motu.
This situation is unfolding and we will continue to update you with further information and plans as they are available.
Ngā mihi
Emma Prestidge (she/her)
Interim Director, Primary, Community and Rural
National Commissioning
waea pūkoro:021 020 25782| īmēra: emma.prestidge@health.govt.nz
Awanui Labs Strike Notice – 20 September
Message on behalf of Awanui Labs:
Awanui Labs have received a notice from APEX of intended strike action by its members for Wednesday 20 September 2023.
This includes a complete withdrawal of labour by all APEX laboratory workers employed by the SCL Group in collection centres and laboratories from 00:00 to 23:59 hours.
Please click here for strike impact information in your region.
Please note that most of the region will be under Life Preserving Services (LPS) this day and approval from a gatekeeper to test will be required. Their contact information and a list of tests approved for LPS will be sent closer to the day. Please do not send any specimens in that do not fall within these criteria. They do not have the ability to store specimens to process the next day.
Aotearoa Immunisation Register (AIR) cut over November 2023
The move from NIR and CIR into AIR is planned for November, with Practice Management Systems (PMS) connecting to the AIR. This will enable practices to record Covid-19 vaccinations into the PMS and ensure all publicly funded vaccinations are recorded in AIR.
If you have any questions or want more information, please see their website, or contact air.engagement@health.govt.nz.
WellSouth in conjunction with the Air Engagement Team will be presenting and updating on the AIR cutover process early October, dates and time to be confirmed.
Shingrix vaccine first dose
We have had a couple of reports of people developing shingles, or herpes zoster, following a first dose of Shingrix.
Shingrix is not a live vaccine so cannot cause shingles. A real-world effectiveness study found that there were around 10 shingles cases for every 1,000 unvaccinated people. This dropped to fewer than five cases per 1,000 among those who received one dose of Shingrix, and dropped to three cases per 1,000 after two doses.
This means some people will develop shingles prior to having their second dose, although their risk is lower than if they had not received the first dose. The data does not suggest an increased risk after dose 1, which is what people may think if they get shingles shortly after the vaccination.
There is evidence that the incidence of herpes zoster is increasing in New Zealand and also that COVID-19 infection increases the risk.
The recommended timing of any dose following an episode of herpes zoster is generally 12 months, as the risk of recurrent shingles is low for about a year after an episode. Those with ophthalmic shingles should wait until 12 months of disease quiescence (has completely settled). Those with immunocompromise could have their second dose sooner than 12 months as they have an increased risk of recurrence.
If you have any questions, please contact 0800 IMMUNE (0800 466 863) or email 0800immune@auckland.ac.nz.
Opportunities to be involved
Survey: Nursing pay gap – impact on services in the community
Working with a number of other concerned organisations, GPLF wishes to raise the profile of the essential role nurses have in primary and community services and build a picture of how the pay gap is driving a nursing workforce shortage which in turn is impacting service provision.
This data is being collected by GPNZ and will be collated and used at a high level for advocacy purposes. Responses will be kept anonymous. Service provision impact data is also being collected from other organisations alongside general practice and primary care.
The survey closes on Monday 18 September.
Complete the survey here.
Update from The Department of General Practice and Rural Health, Dunedin School of Medicine, about changes to the 4th year Medical Students curriculum
Update from Dr Kristin Kenrick
Thank you very much to all those who gave up their time on a Tuesday evening to attend our recent meeting in Dunedin about having 4th Year Medical Students on placement in General Practices. We really appreciated your input, and the meeting has given us plenty to work with as we head into 2024. Invercargill colleagues, you are next on our list to reach out to!
As those who were able to join us will already know, from 2024 the structure of how we teach 4th year students is set to change. We will be moving from our current 5-week module to an 8-week module. This will be the same across the three clinical schools of Otago Medical School and means that we will be able to provide students with a more comprehensive primary care experience. The meeting was largely to discuss how GPs/Practices can contribute to this, and what we in the Department of General Practice and Rural Health can do to make this as straightforward as possible.
Issues that came up for discussion included:
-
Exploring when (and whether or not) payments for having students on placement should go to individual practitioners or to practices.
-
Streamlining our assessment requirements so that these are not unduly burdensome or unrealistic in the setting of a busy general practice.
-
Where possible (and agreed on) utilising other healthcare professionals working in practices to have students spend time with them (e.g. Practice Nurses and Nurse Practitioners, HIPs, HCAs etc.).
-
Making more timeslots available for students to be in practices.
2024
For 2024 we will have 4 x 4-week periods when students are available to be in practices, with consolidated teaching weeks in our department at the beginning and end of each module. Ideally we would like students to spend 16 half-day sessions on placement, but there will need to be some flexibility with this. We will make more than this number of time options available for placement time to assist with this. Note that students will no longer be required to go to ENT clinics during our module.
The dates when student placements are scheduled to occur in 2024 are:
-
-
Group One: 26/02 – 22/03/24
-
Group Two: 29/04 – 24/05/24
-
Group Three: 15/07 – 16/08/24
-
Group Four: 16/09 – 11/10/24
-
We still have a lot of work to do in sorting out timetables, finalising our programme, and getting resources together for those who are hosting our students, but we are committed to keeping General Practices in the loop with what we are planning.
Our main vehicle for communication in the meantime will be via this Newsletter, but please don’t hesitate to contact us directly if you have any questions or concerns. (kristin.kenrick@otago.ac.nz; peter.radue@otago.ac.nz; gprural.admin@otago.ac.nz)
Ngā manaakitanga,
Kristin Kenrick and the GPRH team.
Upcoming training and webinars
CHeST Symposium – Emerging Technologies and Health Systems
Date: 19 September, 9.10am – 5pm
Location: University College (opposite the Business School), University of Otago
Virtual: Hybrid event—you can attend in-person or online—but you must register to attend.
This is the final call to register for this year’s CHeST symposium happening next week.
The theme is “Emerging Technologies and Health Systems”.
Please see the programme booklet for the list of presentations lined up by university researchers and health professionals.
Please register your attendance to this free event by the end of tomorrow using the following link: https://otago.au1.qualtrics.com/jfe/form/SV_b4s2pOA2Ok18uB8
Keynote speakers:
Dr Chris Paton, who will be delivering a seminar on “How can we ensure that new AI-based digital health technologies are safe and effective?”
Dr. Yih Yng (Singapore), who will be discussing “The Hospital without Walls – A Digital Transformation journey of the Tan Tock Seng Hospital”.
Vaccinating Health Worker (VHW) Zoom drop-in session
Date: Thursday 21 September 2023
Time: 12pm-12.30pm
To attend: Please register for the drop-in session here
IMAC and Te Whatu Ora are jointly hosting fortnightly zoom drop-in sessions for Vaccinating Health Workers (VHW), supervisors, employers, and anyone interested in the role as a way to provide support, share information, and address questions related to the VHW workforce and the training pathway.
Participants can benefit from the opportunity to interact with experienced professionals, gain insights into the role, and share information with other providers about the way they utilise the workforce. This drop-in session is 30 minutes.
The panelists are IMAC Education Clinical Advisor Aimee Brass; and Sophie Rapson from Te Whatu Ora’s National Immunisation Programme.
HPV Screening programme
Te Whatu Ora has arranged online drop in sessions so you can ask questions and get support in 'real time' post- 'go live' with two more to go on 15 and 18 September.
Webinar: The scope and impact of Nurse Practitioners
Date: Tuesday 10 October 2023
Time: 7.30pm – 8.45pm
Register here.
Professor Karen Hoare, Nurse Practitioner, Chelsea Wilmott, Nurse Practitioner, Drs Kathryn Smith and Lucy O'Hagan will bring you a practical discussion that covers the essential steps, support, and benefits of this role and how to support your nursing colleagues.
Find out more about the speakers and the agenda here.
ACC training resources
Need a refresher on ACC claiming?
ACC have a suite of education webinars available for health providers looking for an informal way to keep up to date and learn more about working with them.
These popular webinars cover a range of topics across three formats: Beginner’s guides, how-to guides, and special interest topics.
You can register for an upcoming webinar or watch recordings of past webinars on their YouTube playlist on their website here.
Te Whatu Ora update: in case you missed it
Missed the AIR webinar series? Videos are now available to view
The AIR programme has been running a series of webinars since July examining some of the detail on the key shifts the sector will experience when the Aotearoa Immunisation Register (AIR) replaces the National Immunisation Register (NIR) and Covid-19 Immunisation Register (CIR) in November 2023. Recordings of these sessions are available to view here.
You can join the final webinar on Tuesday 19 September by registering here.
Other general information
Pēpi enrolment survey – last chance
There are just two more weeks to share your knowledge and opinions on the process of enrolling newborns in primary care.
Researchers from the University of Auckland the University of Otago are leading a survey to find out the challenges healthcare professionals face when engaging whānau and their pēpi in primary care, with the aim of identifying actions which will support timely immunisation and protection of tamariki Māori from vaccine-preventable diseases.
Anyone working in a general practice or a community setting looking after a newborn's health and the health of their whānau, either in a clinical or non-clinical setting, is encouraged to take part.
The survey results will help inform decisions, policies and practices for the health sector and offer new strategies to address equity gaps.
The survey takes around 10 minutes to complete, and respondents will have the option to go into the draw to win one of five Prezzie cards.
For more information and a link to the survey, please click here.
Covid-19 updates
Last update I forgot to attach the documents regarding the changes to Covid in the Community funding changes, aroha mai. I have attached these to this update. And I have nothing more to say about Covid. For now, at least :)
Funding Guidance for Community Pharmacy Model of Care
Funding Guidance for Primary Care Model of Care
Well, if you’ve made it to the bottom, well done! And I will leave you with a parting thought, made by one wiser than myself, spotted on someone’s wall today.
Have a great week!
Ngā mihi nui
Carol